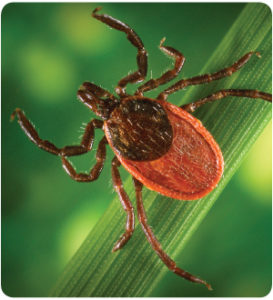
Lyme disease is a tick-borne disease, passed on by the bite of a tick infected by the bacterium Borrelia burgdorferi. The acute symptoms of a recent Lyme disease infection include the appearance of a “bulls-eye” rash at the site of the tick bite along with flu- like symptoms such as fever, joint pains, weakness and fatigue. If caught early enough, an acute Lyme disease infection is often treated very effectively with a course of antibiotics.
Unfortunately it is often the case that symptoms of Lyme disease are mild and thus go unnoticed; and if left untreated, a bite from a borrelia-infected tick will often lead to chronic late-stage Lyme disease, also known as post-Lyme disease syndrome. In these cases, a long term course of antibiotics is usually recommended by medical doctors, even though antibiotics have not been scientifically proven to work in cases of chronic Lyme disease (see “references” at the bottom of the page). In these cases where conventional medical treatment fails, alternative approaches such as homeopathy has proven to be of benefit.
Cases of Chronic Lyme Disease Treated Successfully with Homeopathy
A Case Of Diagnosed Lyme Disease by Tamara Der O’Hanian

Lauren was recovering from Lyme disease for eleven years, prior to her decision to try homeopathy. Over the years, she had taken several rounds of antibiotics and many nutritional supplements. But, Lauren’s recovery had been extremely slow, with major health challenges in the first few years. She was extremely fatigued and needed to sleep several hours each day. Her constant heart pain and palpitations kept her awake at night. Her abilities to think and remember were greatly impaired. She also experienced excruciating burning pains in her abdomen and many joints.
At the time that I met Lauren, she had made progress in her recovery, but she still needed daily naps and felt achy most of the time. Her memory was poor and foggy thinking was a daily reality. As a writer, her hand-eye coordination, something that was automatic, now required effort. Her joints were sore most of the time and she still suffered from weekly abdominal pains.
Within six weeks of taking the homeopathic remedy Spigelia, Lauren reported big improvements. Her energy increased and she only needed to nap once or twice a week. Her thinking was clearer and her memory was slowly recovering. Her pains were less frequent and more tolerable.
Lauren made remarkable progress during her four-month homeopathic treatment. Most of her symptoms disappeared and she was certain that she had made more progress with four months of homeopathic treatment than during the previous eleven years.
A Case of Stage 3, Late Chronic Lyme disease by Ronald D. Whitmont, M.D.

A twenty-six year old female was evaluated in July 2006. She complained of complications resulting from chronic, recurring Lyme disease diagnosed 8 years before. Previously, she had tested positive for Lyme disease, Ehrlichiosis and Babesiosis and had undergone extensive treatment for each of these conditions including extended courses of oral, intravenous and intramuscular antibiotic therapy. Her symptoms now included two “major relapses” annually that included symptoms of hot flashes, gastralgia, arthralgias, anorexia, nuchal rigidity, confusion of sensorium and cognition, difficulty concentrating, and complete exhaustion. Each major relapses typically lasted several months, and were only mitigated by extended courses of oral or intravenous antibiotics.
She also suffered from chronic daily symptoms of severe fatigue and gastrointestinal ill health that included bloating, fullness, easy satiety, post-prandial abdominal distension, frequent belching, nausea, vomiting, muscle cramps, watery diarrhea with mucus, alternating with dry stools and constipation. Her symptoms of early satiety and gastroparesis prevented any weight gain. She had been chronically underweight and malnourished since initiating conventional antibiotic treatment for Lyme.
She had been amenorrheic for 3 years.
The list of medications that had been treated with included Rocephin, Zithromax, mepron, bicillin, Larium, Malarone, doxycycline, flagyl, and various cephalosporins. She had also received treatment reglan and zelnorm. Her current medications included armor thyroid, Claritin and tinidazole.
Over the course of her treatment she had developed a panoply of complications including hypothyroidism, candidiasis, cholelithiasis (leading to cholecystectomy), gastroparesis, intestinal disbiosis, an occular thrombosis with retinal vein occlusion and constipation.
Impression: stage 3 Lyme disease with multi-system involvement and treatment failure using antibiotics.
Treatment: She was treated with the homeopathic medicine Abrotanum artemesia in the Q1 formulation, administered once daily.
First follow up took place one month later in August 2006. At that time, she noted general improvement in all areas. She did note the development of an initial aggravation of her gastrointestinal symptoms that was rapidly followed by increase in her appetite and some modest weight gain.
The next series of follow ups occurred between October and May 2007. She noted continued improvement and stability in all areas. Although this case only has follow up over one year, it is still important since severity and periodicity of her symptoms (which she had experienced for eight years) was immediately altered following homeopathic intervention.
Abrotanum artemisia is known to be associated with malnutrition, emaciation and marasmus. It was selected on the basis of all of her her symptoms at the time of presentation. Treatment in this case followed the patient’s individual manifestations of illness without particular emphasis on the suppressive nature of her previous treatments or the actual diagnosis of Lyme disease. I anticipate that she may need a disease nosode at some point in the future, but the timing of this medicine will be determined by her clinical progress, not by formulae.
A Missed Diagnosis for Mary by Susanne Saltzman, MD
Mary was 14 years old when I saw her in February 1997 for late-stage Lyme disease. She reported having been perfectly healthy until July 1995 when she began to experience symptoms. Her mother said that when Mary first became ill she had a hive-like, itchy rash that waxed and waned, but their pediatrician did not test for Lyme because it did not look like a typical Lyme rash. Mary continued to suffer with the above symptoms on and off for months until her mother took her to another physician who performed a Western Blot test that came back highly positive.
The girl was placed on amoxicillin for one month, and she felt better initially, but her symptoms returned once treatment ended. She began missing school again from continued fatigue, muscle aches, and chronic sore throats. For the next year until I saw her, Mary was placed on a myriad of antibiotics including doxycycline, cefuroxime, and IV rocephin. Each time she received the drugs, she felt better initially only to feel worse again when the treatment was discontinued.
By the time I saw Mary, she was on 7 grams of amoxicillin a day! (A usual dose for more common bacterial infections, such as a middle ear infection, might be 1 to 2 grams per day.) Even so, she complained of many additional symptoms including dizziness, chest pain, constant twitching of her eyelids, extreme sensitivity to light and sound, swollen ankles, and severe migraine headaches. At this point, she had nervous system involvement as evidenced by her extreme sound and light sensitivity, and problems with focusing and short-term memory. An honor student, Mary was very concerned that she was missing so much school.
Mary appeared sweet, shy, and reserved in my office. Her mother described her as very responsible, perfectionistic with her schoolwork, and neat with her possessions. Sitting in front of me was a girl whose case beautifully fit the indications for the homeopathic remedy Natrum muriaticum, as indicated by her emotional sensitivity, reservedness, light sensitivity, and migraines. From my earlier experience treating the boy with late-stage Lyme encephalitis, I suspected that the heavy doses of antibiotics she was taking might interfere with the action of the homeopathic remedy, so I asked Mary’s mother to withdraw them. She was nervous about this but agreed. I explained that Mary might have an aggravation of her symptoms for a day or two after taking the homeopathic remedy, but that they should try not to treat it. I gave Mary Natrum muriaticum 200c.
Within 24 hours of taking the remedy, Mary complained of intense fatigue and a severe migraine—a worsening of her symptoms. By the second day, however, she was feeling better and her symptoms steadily improved over the next several weeks. At her follow-up visit one month later, Mary’s mother stated that for the first 3 weeks, her daughter was back to her old self—happy, energetic, and making jokes at the dinner table. Mary had been completely free of symptoms until just a few days ago when she woke up with a sore throat, fatigue, and headache. I prescribed another dose of Natrum muriaticum 200c. She did well again for two weeks and then relapsed. This pointed to the need for a higher dose, so I gave her Natrum muriaticum 1M. She remained asymptomatic for the next six weeks until she relapsed again. At this point, I gave her Natrum muriaticum 10M.
Mary did great for the next two years! She remained mostly asymptomatic—no headaches, no fatigue, no aches and pains, no chest pain, no dizziness. Her mother was thrilled! The only symptom that remained was ankle swelling when Mary engaged in intense physical activity (she was back on the field hockey team). Then a few of her old symptoms began to creep back… she started to complain of feeling a little fatigued, her headaches returned (though mildly), and her mom said she was getting more irritable. I gave Mary another dose of Natrum muriaticum 10M, and she did beautifully for the next nine years! She is now a 24-year-old medical student.
It is interesting to note that Mary needed several doses of her remedy initially over the course of three months, whereas the boy with Lyme encephalitis was cured with only one dose of his remedy. I suspect that this was because Mary had been on high doses of antibiotics for two years, which probably acted suppressively and weakened her immunity. We can be thankful, however, that the human body has a tremendous capacity for healing, and with the correct homeopathic remedy (as well as a healthy diet, exercise, and a good attitude), people can often spring back from a lifetime of bad habits and/or excessive suppressive therapies and enjoy excellent health and wellness.
Scientific Studies Prove that Antibiotics Do not work for Chronic Lyme Disease
Background
The treatment of persistent symptoms attributed to Lyme disease remains controversial. We assessed whether longer-term antibiotic treatment of persistent symptoms attributed to Lyme disease leads to better outcomes than does shorter-term treatment.
Methods
In a randomized, double-blind, placebo-controlled trial conducted in Europe, we assigned patients with persistent symptoms attributed to Lyme disease — either related temporally to proven Lyme disease or accompanied by a positive IgG or IgM immunoblot assay for Borrelia burgdorferi — to receive a 12-week oral course of doxycycline, clarithromycin plus hydroxychloroquine, or placebo. All study groups received open-label intravenous ceftriaxone for 2 weeks before initiating the randomized regimen. The primary outcome measure was health-related quality of life, as assessed by the physical-component summary score of the RAND-36 Health Status Inventory (RAND SF-36) (range, 15 to 61, with higher scores indicating better quality of life), at the end of the treatment period at week 14, after the 2-week course of ceftriaxone and the 12-week course of the randomized study drug or placebo had been completed.
Results
Of the 281 patients who underwent randomization, 280 were included in the modified intention-to-treat analysis (86 patients in the doxycycline group, 96 in the clarithromycin–hydroxychloroquine group, and 98 in the placebo group). The SF-36 physical-component summary score did not differ significantly among the three study groups at the end of the treatment period, with mean scores of 35.0 (95% confidence interval [CI], 33.5 to 36.5) in the doxycycline group, 35.6 (95% CI, 34.2 to 37.1) in the clarithromycin–hydroxychloroquine group, and 34.8 (95% CI, 33.4 to 36.2) in the placebo group (P=0.69; a difference of 0.2 [95% CI, –2.4 to 2.8] in the doxycycline group vs. the placebo group and a difference of 0.9 [95% CI, –1.6 to 3.3] in the clarithromycin–hydroxychloroquine group vs. the placebo group); the score also did not differ significantly among the groups at subsequent study visits (P=0.35). In all study groups, the SF-36 physical-component summary score increased significantly from baseline to the end of the treatment period (P<0.001). The rates of adverse events were similar among the study groups. Four serious adverse events thought to be related to drug use occurred during the 2-week open-label ceftriaxone phase, and no serious drug-related adverse event occurred during the 12-week randomized phase.
Conclusions
In patients with persistent symptoms attributed to Lyme disease, longer-term antibiotic treatment did not have additional beneficial effects on health-related quality of life beyond those with shorter-term treatment.
Objective: To determine whether post Lyme syndrome (PLS) is antibiotic responsive.
Methods: The authors conducted a single-center randomized double-masked placebo-controlled trial on 55 patients with Lyme disease with persistent severe fatigue at least 6 or more months after antibiotic therapy. Patients were randomly assigned to receive 28 days of IV ceftriaxone or placebo. The primary clinical outcomes were improvement in fatigue, defined by a change of 0.7 points or more on an 11-item fatigue questionnaire, and improvement in cognitive function (mental speed), defined by a change of 25% or more on a test of reaction time. The primary laboratory outcome was an experimental measure of CSF infection, outer surface protein A (OspA). Outcome data were collected at the 6-month visit.
Results: Patients assigned to ceftriaxone showed improvement in disabling fatigue compared to the placebo group (rate ratio, 3.5; 95% CI, 1.50 to 8.03; p = 0.001). No beneficial treatment effect was observed for cognitive function or the laboratory measure of persistent infection. Four patients, three of whom were on placebo, had adverse events associated with treatment, which required hospitalization.
Conclusions: Ceftriaxone therapy in patients with PLS with severe fatigue was associated with an improvement in fatigue but not with cognitive function or an experimental laboratory measure of infection in this study. Because fatigue (a nonspecific symptom) was the only outcome that improved and because treatment was associated with adverse events, this study does not support the use of additional antibiotic therapy with parenteral ceftriaxone in post-treatment, persistently fatigued patients with PLS.
Background
It is controversial whether prolonged antibiotic treatment is effective for patients in whom symptoms persist after the recommended antibiotic treatment for acute Lyme disease.
Methods
We conducted two randomized trials: one in 78 patients who were seropositive for IgG antibodies to Borrelia burgdorferi at the time of enrollment and the other in 51 patients who were seronegative. The patients received either intravenous ceftriaxone, 2 g daily for 30 days, followed by oral doxycycline, 200 mg daily for 60 days, or matching intravenous and oral placebos. Each patient had well-documented, previously treated Lyme disease but had persistent musculoskeletal pain, neurocognitive symptoms, or dysesthesia, often associated with fatigue. The primary outcome measures were improvement on the physical- and mental-health–component summary scales of the Medical Outcomes Study 36-Item Short-Form General Health Survey (SF-36) — a scale measuring the health-related quality of life — on day 180 of the study.
Results
After a planned interim analysis, the data and safety monitoring board recommended that the studies be discontinued because data from the first 107 patients indicated that it was highly unlikely that a significant difference in treatment efficacy between the groups would be observed with the planned full enrollment of 260 patients. Base-line assessments documented severe impairment in the patients’ health-related quality of life. In intention-to-treat analyses, there were no significant differences in the outcomes with prolonged antibiotic treatment as compared with placebo among either the seropositive or the seronegative patients.
Conclusions
There is considerable impairment of health-related quality of life among patients with persistent symptoms despite previous antibiotic treatment for acute Lyme disease. However, in these two trials, treatment with intravenous and oral antibiotics for 90 days did not improve symptoms more than placebo.
The authors of four National Institutes of Health (NIH)-sponsored antibiotic treatment trials of patients with persistent unexplained symptoms despite previous antibiotic treatment of Lyme disease determined that retreatment provides little if any benefit and carries significant risk. Recently, two groups have provided an independent reassessment of these trials and concluded that prolonged courses of antibiotics are likely to be helpful. We have carefully considered the points raised by these groups, along with our own critical review of the treatment trials. Based on this analysis, the conclusion that there is a meaningful clinical benefit to be gained from retreatment of such patients with parenteral antibiotic therapy cannot be justified.
